The authors of a new study under review at Nature Portfolio and currently posted to the Research Square preprint* server showed the clinical possibility that the coronavirus disease 2019 (COVID-19) heightens the risk of developing diabetes mellitus (DM), supporting diabetes screening in those infected by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
 Study: New-Onset Diabetes and COVID-19: Evidence from a Global Clinical Registry. Image Credit: ADragan / Shutterstock
Study: New-Onset Diabetes and COVID-19: Evidence from a Global Clinical Registry. Image Credit: ADragan / Shutterstock
Background
An increasing body of evidence suggests that COVID-19 is associated with new diabetes diagnoses. However, it is unclear whether COVID-19 detects pre-existing diabetes or induces new-onset diabetes.
Although previous research reported high blood-sugar levels and metabolic consequences resulting from pre-existing diabetes following COVID-19 hospitalization, studies correlating the disease to new-onset DM are scarce.
COVID-19 has been shown to exacerbate pre-existing diabetes. This likely occurs because COVID-19 is associated with low-grade inflammation, which may initiate or worsen insulin resistance. In addition, numerous studies have also demonstrated that SARS-CoV-2 can infest and multiply within insulin-producing pancreatic beta-cells, thus impairing insulin synthesis and secretion.
However, whether SARS-CoV-2 can cause clinically meaningful changes in glucose metabolism remains unclear. Nevertheless, it may be possible to find an answer by characterizing the clinical symptoms of COVID-19-related diabetes and by determining the period between the onset of hyperglycemia and that of the infection.
It is imperative to establish a causal relationship between COVID-19 and diabetes since both diseases are prevalent throughout the world. Furthermore, establishing a causal relationship will have significant implications for diagnosis, management, public health, and scientific research. Despite this, it remains unclear whether the association between COVID-19 and diabetes results from indirect health consequences of the former, such as – a higher rate of detection of pre-existing diseases, or whether the causative virus (SARS-CoV-2) directly precipitates hyperglycemia.
Owing to the higher rate of pre-existing disease detection in the COVID era, newly diagnosed diabetes may be explained both during and after an episode of infectious exposure.
The study
This study investigated the possibility that COVID-19 may trigger new-onset diabetes and its associated symptoms by examining average blood-glucose levels at the time of diabetes presentation against a global clinical registry.
A global COVID-19-related diabetes (CoviDIAB) registry was established to determine whether COVID-19 can acutely induce diabetes and its clinical symptoms. The CoviDIAB registry collects information regarding “newly diagnosed diabetes” and “severe metabolic complications associated with pre-existing diabetes” resulting from COVID-19.
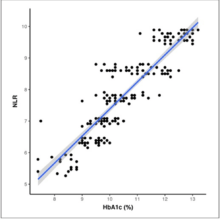
Individuals with a fasting blood glucose of 126 mg/dL or above or non-fasting blood glucose of 200 mg/dL or above, with no prior diabetes history, and those who had never been on glucose-lowering medications, and with their glycated hemoglobin (HbA1c) levels below the diabetic range (< 6.5%) at presentation were categorized as new-onset diabetes. Here, the researchers examined cases of newly diagnosed diabetes that occurred within four weeks of COVID-19 confirmation. In addition, the HbA1c data were evaluated at the time of diabetes detection to rule out pre-existing hyperglycemia and to confirm the association with SARS-CoV-2 infection.
The findings
Data on 537 eligible newly diagnosed diabetes cases was entered from 61 hospitals in 25 countries between 2020-2022. COVID-19 patients with newly diagnosed diabetes at presentation had HbA1c levels above the diagnostic range, suggesting pre-existing hyperglycemia.
In cases with new-onset hyperglycemia after the SARS-CoV-2 infection, individuals displayed glycemic levels above the diagnostic thresholds, although their HbA1c levels remained within the non-diabetic range. The results showed that 22% of newly diagnosed patients with documented HbA1c levels had recently acquired diabetes.
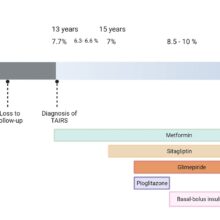
The most common diabetes subtype among adults was type 2 DM (59%), and the “not yet known” subtype (41%). Two newly diagnosed cases of type 1 DM were recorded among children. After COVID-19 resolution, hyperglycemia persisted in 39 of 89 patients (45%) with newly diagnosed diabetes.
For 28 of these individuals, follow-up data beyond three months was collected, demonstrating that five of them were in remission from diabetes, while 23 (82%) remained diabetic.
The findings suggested that COVID-19 causes clinically significant changes in glucose metabolism. Although this study does not prove that SARS-CoV-2 causes diabetes, it strongly suggests that the virus may impose a diabetogenic aftermath.
Further, type 2 DM was the predominant subtype among COVID-19 participants with newly diagnosed diabetes. Thus, type 2 DM likely accounts for most newly diagnosed diabetes cases associated with the post-acute phase of the SARS-CoV-2 infection.
This study confirms this phenomenon across diverse geographical locations and ethnicities by incorporating clinical observations from 25 countries.
Numerous areas for improvement have been identified in this study, including inherent heterogeneity in clinical practice and the judgment of contributing physicians.
Conclusion
The results of this study suggest that COVID-19 likely has a diabetogenic effect. Thus, individuals exposed to SARS-CoV-2 infection must be screened for diabetes. Further research is necessary to confirm the mechanisms through which the virus interferes with glucose metabolism.
*Important notice
Research Square publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.